Introduction
Femoroacetabular impingement (FAI) and its management continues to be a controversial subject. As physiotherapists, we need to provide patients and surgeons with high quality, efficacious treatment alternatives to surgery. The focus of this editorial is to review the pathoanatomy of FAI and discuss new research comparing physiotherapy to surgery. Finally, using our evolving evidence base, discuss guidelines for best future practice to ensure optimal patient care.
The Warwick Agreement
FAI was originally conceptualized solely from a morphological and mechanical perspective, defined as the abnormal, premature, osseous contact between the proximal femur and/or the acetabular rim during end-range hip motions. Confusion surrounding this definition, specifically its relevance to asymptomatic individuals, prompted an international consensus meeting in 2016 with world experts led by orthopaedic surgeon Damien Griffin (1). Known as the Warwick agreement, this consensus statement has provided more clarity and led to a more clinically relevant definition entitled “FAI syndrome (FAIS)”. Importantly, FAIS diagnosis requires a triad of 1). symptoms, 2). clinical findings and 3). radiological findings, as opposed to imaging alone.
Morphology, Pathology, and OA.
There are 3 types of FAI morphology:
- Cam describes an extra bone growth most prevalent on the anterior, superio
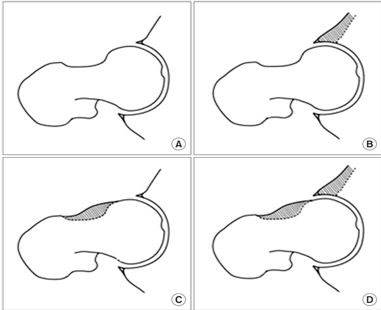
Impingement Morphology
r and anterosuperior aspect of the femoral head-neck junction (Figure 1C). This is the most common morphology.
- Pincer (Figure 1B) describes an extra bone growth on the acetabulum.
- Mixed describes when both cam and pincer are present (Figure1D).
Clinicians need to be aware of the different anatomical variants as the type of morphology may influence intervention options and future prognosis (2). It is also important to recognize that in isolation morphology is not a medical finding or a pathology and is only relevant in patients who are symptomatic. Having said this, we must be aware that hips with cam morphology are at higher risk of OA development and between 6% and 25% will develop future OA within 5 to 19 years (3). A cam morphology is defined as an alpha angle >60° and a cam >83° further increases a patient’s risk of OA (4). Although these statistics often promote an element of fear around cam morphology, it must be remembered the majority of people with cam morphology will not develop OA.
Surgery vs Conservative Management: Recent Research.
The optimal management of patients with FAIS is still largely unknown. However, two significant papers were published in 2018 comparing hip arthroscopy to physiotherapy. Mansell et al (5) compared hip arthroscopy (n=38) to physical therapy (n=40) in military personnel. The study used the Hip Outcome Score (HOS) as their primary outcome measure and the iHot33 and Global Rating of Change (GROC) as their secondary outcome measures. They assessed outcomes at 6 months, 1 year and 2 years. Both groups improved, however, no significant difference was found between groups at 2 years. Unfortunately, 28% of the physiotherapy group ended up having surgery and due to this large crossover, a degree of ambiguity remains around the results. Worryingly, 58.1% of all participants did not perceive a clinically meaningful change at two years and 1/3 of participants were not fit for active duty. Griffin et al (6) performed a large RCT called the FASHIon trial comparing hip arthroscopy (n=171) to conservative care (n=177) using the iHot33 as their primary outcome measure at 6 and 12 months post-intervention. Similar to Mansell, both groups improved with the surgical group demonstrating a slightly better outcome (iHot33 6.8pts).
What This Tells Us.
These research studies indicate that both surgery and physiotherapy help people with FAIS but we are not sure what the natural history is in these populations as no study has been compared to no intervention or sham. On average, patients are left with only moderate hip-related quality of life scores irrespective of the intervention (50-60/100 iHot33). It should be noted that both groups found slightly better QOL outcomes with surgery. Unfortunately, it is difficult to solely associate this outcome with the surgery, as both group also received extensive post-op physiotherapy. Finally, the surgical group in the FASHIon trial reported 5 adverse events and a joint infection and one has to question if an extra 6.8pts on the iHot33 (MCID = 6.1 (7) & 10 (8)) is worth the risks and costs associated with surgical intervention.
Guidelines for Best Practice: Physio First, Treat the Individual.
With current evidence, physiotherapy should be the first treatment approach for patients with FAIS. Before beginning an intervention, it is imperative as part of a shared decision-making process that we acknowledge the patient’s individual values and specific goals, be it from activities of daily living to returning to high-level sport. A crucial element of early management is education. This should include load management, awareness of impingement positions, pathology, prognosis and treatment options. We need to explain that currently, the efficacy of both physiotherapy and surgical interventions is limited and QOL post both interventions is only moderate. Similarly, in some patients, physiotherapy may fail, and patients may require a surgical opinion. As previously mentioned, although the majority of patients will not develop hip OA, FAI is a risk factor. This needs to be explained to patients in a non-threatening way and they need to be given proactive life-long advice such as weight loss, general exercise and specific exercise to help reduce OA risk.
A primary goal when treating FAIS is to optimize hip joint loads using current knowledge of impairments in this cohort. An impairment based rehabilitation program for FAI should address known deficits in muscle strength, range of motion and altered gait and functional movement patterns (9). As well as physical impairments, we need to utilize our clinical reasoning as part of a wider biopsychosocial approach to tailor individualized rehabilitation programs to the patient in front of us. Westermann et al (10) found that factors such as mental health, activities levels, sex, and smoking were more predictive of baseline hip pain and function than were intra-articular findings during hip arthroscopy for FAIS. In a condition that is heavily pathoanatomically and mechanically focused, let’s not forget about psychosocial factors.
References
- Griffin D, Dickenson E, O’donnell J, Awan T, Beck M, Clohisy J, et al. The Warwick Agreement on femoroacetabular impingement syndrome (FAI syndrome): an international consensus statement. Br J Sports Med. 2016;50(19):1169-76.
- Van Klij P, Heerey J, Waarsing JH, Agricola R. The prevalence of cam and pincer morphology and its association with development of hip osteoarthritis. journal of orthopaedic & sports physical therapy. 2018;48(4):230-8.
- Heijboer MP, Bierma-Zeinstra SM, Verhaar JA, Weinans H, Waarsing JH. Cam impingement causes osteoarthritis of the hip: a nationwide prospective cohort study (CHECK). Annals of the rheumatic diseases. 2012:annrheumdis-2012-201643.
- Waarsing J, Thomas G, Carr AJ, Reijman M, Bierma-Zeinstra S, Glyn-Jones S, et al. Cam impingement: defining the presence of a cam deformity by the alpha angle: data from the CHECK cohort and Chingford cohort. Osteoarthritis and cartilage. 2014;22(2):218-25.
- Mansell NS, Rhon DI, Meyer J, Slevin JM, Marchant BG. Arthroscopic surgery or physical therapy for patients with femoroacetabular impingement syndrome: a randomized controlled trial with 2-year follow-up. The American journal of sports medicine. 2018;46(6):1306-14.
- Griffin DR, Dickenson EJ, Wall PD, Achana F, Donovan JL, Griffin J, et al. Hip arthroscopy versus best conservative care for the treatment of femoroacetabular impingement syndrome (UK FASHIoN): a multicentre randomised controlled trial. The Lancet. 2018;391(10136):2225-35.
- Mohtadi NG, Griffin DR, Pedersen ME, Chan D, Safran MR, Parsons N, et al. The development and validation of a self-administered quality-of-life outcome measure for young, active patients with symptomatic hip disease: the International Hip Outcome Tool (iHOT-33). Arthroscopy. 2012;28(5):595-610. e1.
- Kemp JL, Collins NJ, Roos EM, Crossley KM. Psychometric properties of patient-reported outcome measures for hip arthroscopic surgery. The American journal of sports medicine. 2013;41(9):2065-73.
- Freke MD, Kemp J, Svege I, Risberg MA, Semciw A, Crossley KM. Physical impairments in symptomatic femoroacetabular impingement: a systematic review of the evidence. Br J Sports Med. 2016;50(19):1180-.
- Westermann RW, Lynch TS, Jones MH, Spindler KP, Messner W, Strnad G, et al. Predictors of hip pain and function in femoroacetabular impingement: a prospective cohort analysis. Orthopaedic journal of sports medicine. 2017;5(9):2325967117726521.